The last two days of the Sydney hearing kept up the theme of medical restraints in aged care. Josef Ibrahim spoke at length on psychotropic misuse and we also heard from Christina Bolger, executive director, regulatory policy and performance at the Aged Care Quality and Safety Commission, and previously at the Australian Aged Care Quality Agency.
She extolled the virtues of the safety commission and a new measure in pilot, ready by 2020, which is a “risk-profiling instrument” that will assess “the performance and compliance of individual services at the sector".
It will also profile risk that might be relevant to particular consumers within the service in conjunction with the new quality framework coming into effect on July 1.
The safety commission has encountered increased noncompliance around the use of psychotropics. According to Bolger, this is due to better detection methods and unannounced re-accreditation audits. All re-accreditation audits are now unannounced, which means that the providers have no notice of the day that the quality assessment team will arrive.
However, counsel assisting Peter Gray appeared to disagree with Bolger as to whether the new audits are, in fact, better than before.
“If it’s just the case that if information of concern about compliance with those expected outcomes is found during a visit, then a review audit might result. Isn’t that the way it has always been at the agency?” probed Gray.
“I would suggest that it is, because we’re actually making better use of that information,” Bolger replied. "And part of that is the use of the complaints data. And having integrated the complaints function into the commission from 1 January this year has meant that we have stronger line of sight to the complaints information, which, again, is a form of intel for the commission.
“Previously, the quality agency relied on referrals to the quality agency. And, whilst those referrals had been increasing, having that information available in a single entity is enhancing our understanding of risk.”
Bolger did concede that a big part of quality assurance involves asking questions of the consumer, and when dealing with those with cognitive impairment this might be hard to ascertain, especially when it comes to restraint in the form of over-medication.
Final thoughts
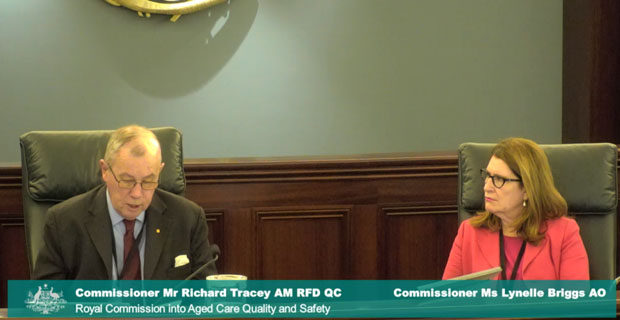
At the start of the final day's testimony, commissioner Richard Tracey felt the need to repeat his remarks from January regarding the safety of those coming forward to testify.
“Under section 6M of the Royal Commissions Act it is a criminal offence for a person to injure another who has appeared as a witness or produced a document or given information or a statement pursuant to a summons requirement or notice issued by the royal commission,” he said.
“Let there be no doubt, the Royal Commission will not hesitate to take steps within its powers to ensure that witnesses and those otherwise engaging with us are protected in accordance with the Royal Commissions Act or the common law."
We heard from Henry Brodaty, professor at UNSW, who said nursing homes currently do not do enough to facilitate GP visits.
Typically, he said, GPs go to a home then have to spend time finding the patient, finding a nurse, finding the medication notes, and for a GP who gets a small amount of money for these visits, “it’s not very attractive for them and it’s very inefficient use of their time, and every minute is how they support themselves".
The commission ended with testimony from witnesses with younger onset dementia.
Trevor Crosby was diagnosed with Lewy body dementia four years ago at age 65. He and his family and friends noticed a change in his personality over a period of time. He went from “the leader of the pack” to someone who “started dropping off to be at the back of the pack,” and initially he put this down to older age.
“The very first moment that I found out, I tried to speak, but I couldn’t. I really understood what the definition of speechless was. I choked. I cried," he said.
Crosby lamented the lack of support people like he and his wife, Jill, are afforded once they receive a diagnosis.
He told the commission about the living with dementia program he undertook with Dementia Australia, which he described as a “real turning point” for him and Jill.
However, after the eight-week course he felt cut adrift.
“Eight weeks just wasn’t enough, isn’t enough. After I completed the course, I felt cheated. The course was so good, but there was no follow-up … There was no second instalment. I didn’t want it to end,” he said.
However, he told the commission that in some ways, his diagnosis has changed his life for the better.
“That I have dementia has increased my quality of life, would you believe.
“It has helped me face the evil monster and seek out the true priorities of life. I make time for my true friends and doing things that make me happy, spending time with my family and caring dear friends, golf, yoga... eating well, speaking out about dementia."
The last witness of the Sydney hearing was academic and chair and chief executive of Dementia Alliance International, Kate Swaffer.
Swaffer was diagnosed with a rare form of younger onset dementia 10 years ago, aged just 49.
She told the commission that it wasn’t until 12 months into her diagnosis that she was referred to support services, which in her words “set us up to fail”.
“It told me that I wasn’t changing. It told [my partner] that I was changing, and it mostly talked about behaviours to expect and advised me to get my end of life affairs in order and to get acquainted with aged care.”
People diagnosed with dementia need “intensive brain injury rehabilitation,” and for people of her age to be “supported to stay at work with reasonable accommodations,” just as if she had suffered an accident causing brain injury.
The next public hearing of the royal commission will be from 17 to 19 June in Broome, WA, and then from 24 to 28 June in Perth. The focus of this next hearing will be on aged care for Indigenous Australians, person-centred care and the delivery of aged care in remote locations.
Click here for more on the royal commission.
Do you have an idea for a story?Email [email protected]
 Aged Care Insite Australia's number one aged care news source
Aged Care Insite Australia's number one aged care news source