A new trial has found an antibiotic did not protect against infection and instead may have led to more infections and adverse reactions in patients.
Currently, cefazolin is used as an antibiotic to prevent infection immediately after surgery.
But with the rise of antibiotic-resistant bacteria, experts have debated whether adding a second antibiotic, vancomycin, would be better to prevent more infection.
Many centres around Australia have adopted using both cefazolin and vancomycin to prevent infections – despite the lack of clear benefits.
The trial, led by researchers at Monash University, looked at over 4,000 patients across 11 hospitals in Australia.
Patients were randomly selected to receive either vancomycin or a saline placebo, combined with cefazolin.
The trial found the addition of vancomycin was no better than the cefazolin antibiotic.
Unexpectedly, patients undergoing knee joint replacements had a higher risk of infection, with the vancomycin group at 5.7 per cent compared to the placebo group at 3.7 per cent.
Professor Trisha Peel, the study's lead researcher, said the trial answered an important question.
"Given the number of joint replacements performed in Australia, our trial has answered the important question about whether more antibiotics are better for our patients having joint replacement surgery," Professor Peel said.
"With the definitive answer being 'no', this trial will have a significant impact on practice."
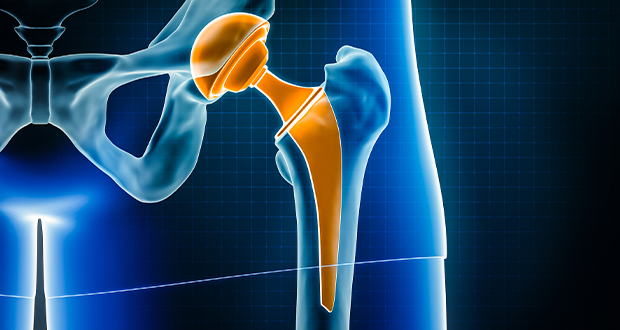
Knee and hip replacements are on the rise due to an increase in the ageing population.
Since 1999, there have been over 1.5 million joint replacement procedures, with 22.5 per cent of older Australians requiring one.
With the aging population set to triple in size over the next 40 years, knee and hip replacements will rise respectively by 276 and 208 per cent – costing the healthcare system $5.32 billion.
Post-surgery infections, while rare at one to five per cent of patients, result in high patient morbidity and mortality – costing Australian hospitals over $21,000 per infection, adding an extra $97 million to healthcare costs.
Following the results of the trial, Professor Peel said it was always necessary to conduct large clinical trials, which helps in re-evaluation.
"A lot of things seem to make sense, but we don't really know for sure until they are tested in a clinical trial," she said.
"This is one of those cases – more antibiotics weren't better, and in some people, might actually be worse."
Do you have an idea for a story?Email [email protected]
 Aged Care Insite Australia's number one aged care news source
Aged Care Insite Australia's number one aged care news source